Report: China's fight against COVID-19 (full text)
III. Screening, testing and dynamic monitoring
Screening, testing and monitoring with epidemiological investigation at the core became a key approach to cut virus transmission and provide timely treatment to infected patients.
China laid great stress on epidemic control and prevention at the source, and implemented policies of "early detection, early reporting, early isolation and early treatment" and "testing all who need to be tested, hospitalization of all who need to be hospitalized, isolating and treating all who need to be isolated and treated". Of the policies, "early detection and early reporting" and "testing and isolating all in need" were a priority, which played an important role in reducing transmission and fatality rates.
1. Thorough screening at communities
— Considering that more than 80 percent of all infections occurred in communities, authorities in Wuhan dispatched more than 80,000 government employees to conduct a thorough survey of all households in the city, which number more than 4 million. Various means such as personal visits, telephone calls and the internet were used. As a result, all confirmed and suspected cases, and those who had close contact with confirmed cases in communities were identified and transferred to hospitals or other designated places, which helped ensure the elimination of potential sources of infection in communities.
— Nationwide, comprehensive screening in communities was done in all provinces, autonomous regions and municipalities, and door-to-door visits were combined with voluntary checks and reporting by residents. All confirmed and suspected cases, suspected cases with fever, those who had close contact with confirmed cases and residents who returned from badly-hit epidemic areas were registered. All confirmed cases were hospitalized, and those displaying fever symptoms were sent to designated venues for isolation and medical observation, while those who had close contact with confirmed patients were sent to designated quarantine sites such as hotels for medical observation. Later, all people coming from overseas were subject to isolation at designated quarantine sites.
2. Improving virus testing
— Testing was done on all people in need as soon as possible with improved supply of testing kits. With increased production of testing kits, the initial short supply was overcome in the shortest period of time. Authorities expanded the list of institutes certified to conduct such tests by allowing P2 biosafety labs, qualified major hospitals, centers for disease control and prevention and professional testing institutes that could carry out reverse transcription polymerase chain reaction to provide nucleic acid tests so that all suspected cases could be tested. As a result, the daily testing capacity in Hubei province increased from 300 samples at the beginning of the outbreak to more than 20,000, with certified institutes providing round-the-clock testing services.
— Shortening testing cycle and ensuring quality
Initially, slow nucleic acid testing led to difficulties in patients being diagnosed and admitted to hospitals. Testing procedures were streamlined and more institutes authorized to give such tests. As a result, cases did not have to be reviewed by the Chinese Center for Disease Control and Prevention for confirmation, except cluster cases, to reduce the time needed to confirm infections. Therefore, the test cycle of the virus reduced from six days at the beginning of the outbreak to between four and six hours, and even shorter, later.
Across the rest of the country too, nucleic acid test labs were set up, training for testing workers and managerial staff was stepped up, and improved quality control systems were set in place to improve virus testing ability and ensure precise results.
As most suspected cases display pneumonia-like computed tomography images, clinically diagnosed cases were temporarily considered as confirmed so that they could receive treatment. The measure raised the cure rate of infected patients and reduced the mortality rate.
3. Establishing a dynamic management system
— China promoted an epidemic control and prevention strategy with tailored measures for different areas, and all county-level areas were categorized as low-risk, medium-risk or high-risk based on their population and degree of epidemic prevalence. Low-risk areas took strict measures to prevent imported cases, while getting ready to resume normal life and economic activity. In medium-risk areas, measures were taken to both prevent imported cases and spread of the virus, with resumption of work and production proceeding in an orderly manner. High-risk areas focused their efforts on control and prevention, preventing cases from being exported to other areas and halting the spread of the virus within its own area.
— The focus of epidemic control and prevention was constantly adjusted to meet new challenges such as preventing imported cases and domestic re-infections. A joint-work mechanism comprising different departments such as aviation, customs, public security, health, foreign affairs, border inspection and airports was established to prevent transmission of the virus at the point of first entry. With an increasing number of asymptomatic cases, it was decided to place all such cases under medical observation in isolation for 14 days at designated sites, and allow them to be discharged only after they test negative twice consecutively.
— Health QR codes were promoted to ensure convenience for residents. Individuals could download health QR codes from government service network platforms to serve as permits for making trips, going to school or work, daily life and accessing public venues. The codes are in three colors — green, yellow and red — and so restrictions could be imposed accordingly. This way, data on epidemic control could be collected precisely.
4. Intensifying epidemiological investigation
— Epidemiological teams were set up to precisely trace and cut off transmission channels. Big data technology and digitalized systems were used to improve preciseness and efficiency of epidemiological investigations. Tracing those who had close contact with confirmed patients was key so that all cases were detected as early and quickly as possible. All asymptomatic cases and those who had close contact with confirmed cases were put under medical observation. During the peak of the epidemic, 1,800 epidemiological groups were set up with five members in each team to thoroughly investigate the movement history of confirmed cases and their close contacts.
— Surveys were conducted among focus groups of people and in key areas, confirmed cases, suspected cases, asymptomatic cases and cluster cases that were identified at various medical institutions, communities and households could be traced and investigated. Abnormal cases found at enterprises that had resumed production and at schools and kindergartens that reopened as well as in nursing homes for elderly people and facilities for the disabled could also be traced and investigated. During the later stages of the epidemic, confirmed cases and their close contacts, suspected cases and people from overseas displaying symptoms of fever were also traced and investigated.
— Tailored epidemiological investigations were organized to target asymptomatic cases in Hubei province, including its capital Wuhan, and some other provinces. Epidemiological surveys were completed within 24 hours for every asymptomatic case identified. Evaluation was made on whether asymptomatic cases would transmit the virus to other people and the result was made public; in the latter period of the outbreak, a serum antibody epidemiological survey was initiated to provide scientific evidence for targeted control.
5. Handling four groups for specific treatment
— Confirmed patients were hospitalized for treatment based on their conditions as early as possible. Serious patients were sent to designated hospitals for treatment, while those with mild symptoms were sent to designated facilities, including makeshift hospitals, for treatment under isolation.
— Suspected cases were given treatment based on their condition or placed under observation in quarantine. Suspected cases were sent to hospitals for treatment if they were in serious condition, while those with mild symptoms were sent to designated places for isolation if they could not be admitted to hospitals. Cases that tested negative for the virus twice but exhibited clinical symptoms were treated as suspected cases.
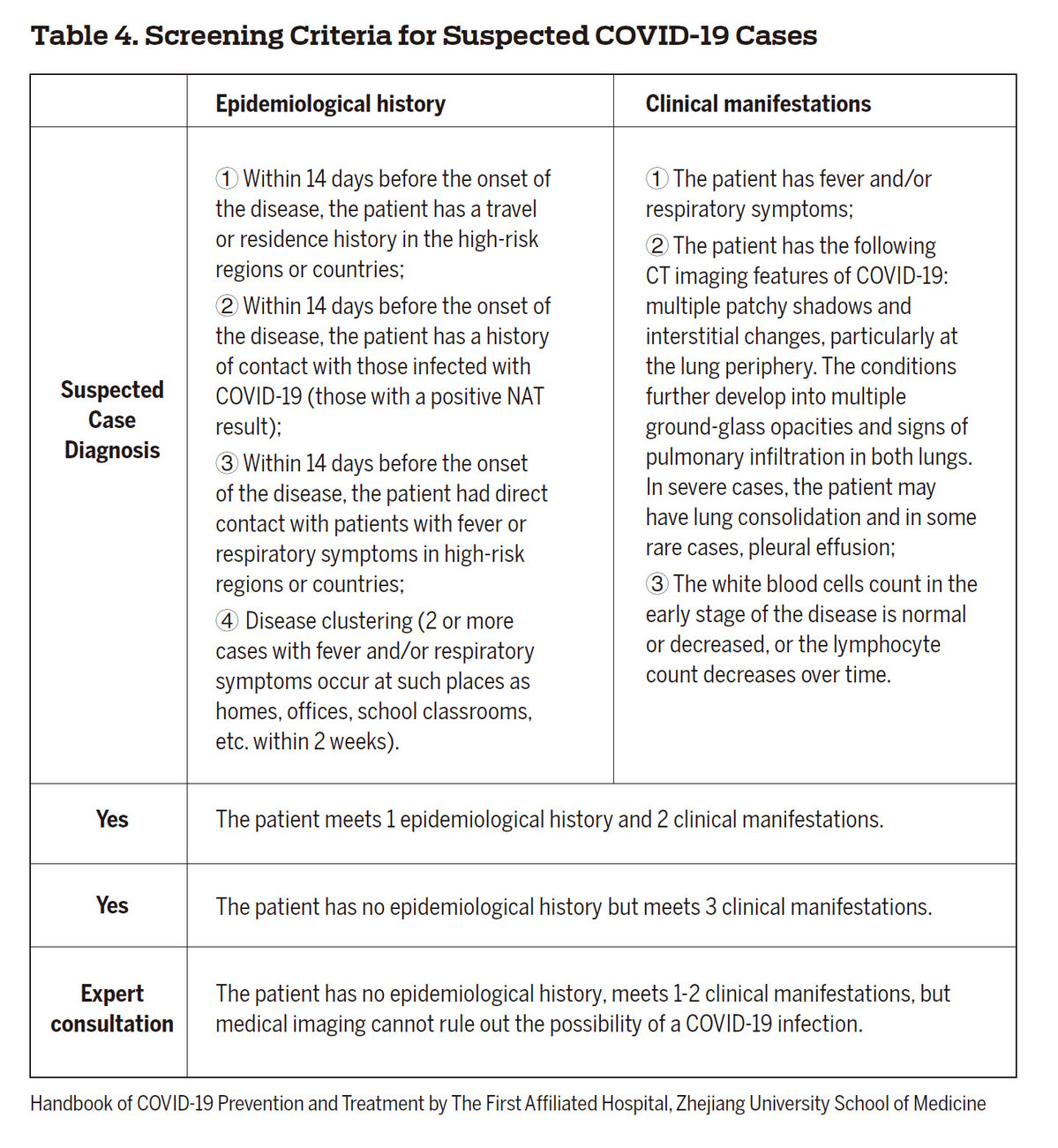
— Those with fever were placed under observation in isolation. Fever patients who could not be ruled out to be COVID-19 cases were treated as suspected cases and put under observation in isolation at designated places, but were separated from suspected cases to prevent possible cross-infection.
— Close contacts of confirmed cases were put under observation in isolation at designated places. Some of them may have been asymptomatic but infected so they were put under observation in isolation at designated places.
Please feel free to contact us by sending your questions to question@chinadaily.com.cn or commenting on China Daily app. We will ask experts to answer them.